Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs. Therefore, doctors often classify ulcerative colitis according to its location.
You may have the following signs and symptoms, depending on which part of the colon is inflamed:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- Rectal pain
- Rectal bleeding — passing small amount of blood with stool
- Urgency to defecate
- Inability to defecate despite urgency
- Weight loss
- Fatigue
- Fever
- In children, failure to grow
Most people with ulcerative colitis have mild to moderate symptoms. The course of ulcerative colitis may vary, with some people having long periods of remission.
Contents
Types
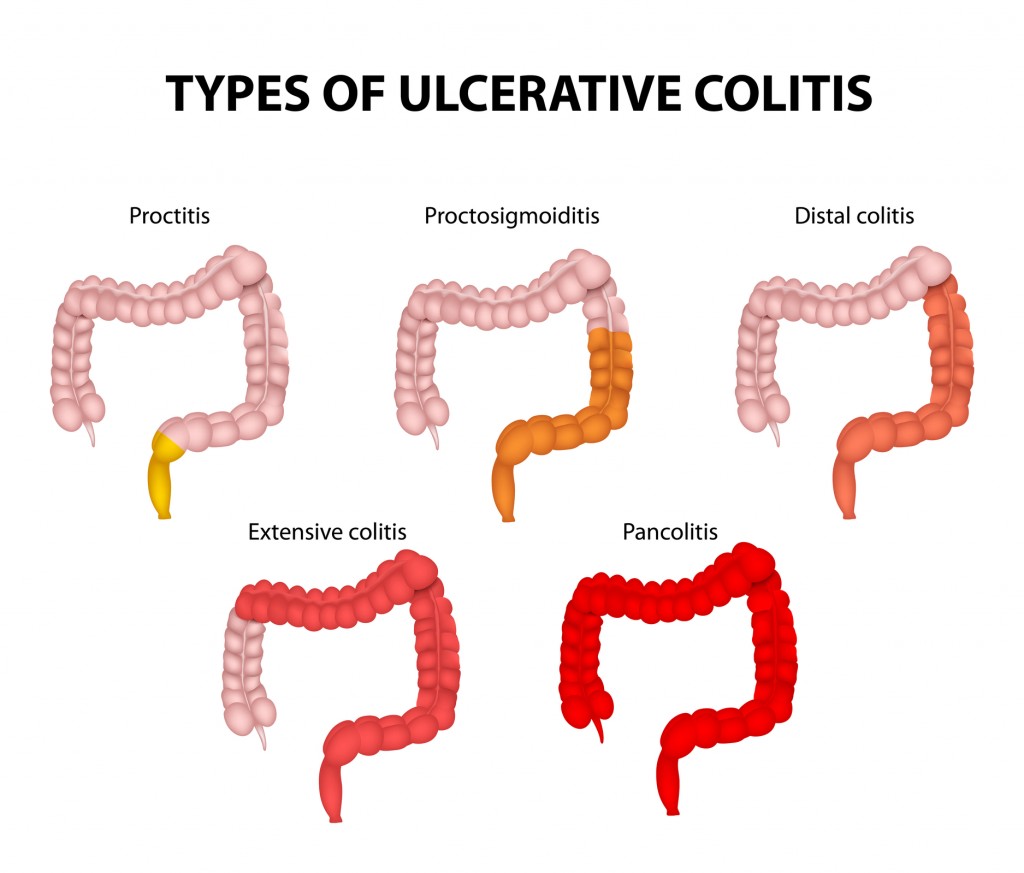
Ulcerative colitis is classified according to how much of your colon is affected. The condition can be mild and limited to the rectum (ulcerative proctitis). Or it can affect additional parts of your colon, generally with more severe symptoms. People who develop ulcerative colitis at a younger age are more likely to have severe symptoms.
Symptoms of ulcerative colitis
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- abdominal (tummy) pain
- needing to empty your bowels frequently
You may also experience fatigue (extreme tiredness), loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is. For some people, the condition has a significant impact on their everyday lives.
Symptoms of a flare-up
Some people may go for weeks or months with very mild symptoms, or none at all (known as remission), followed by periods where the symptoms are particularly troublesome (known as flare-ups or relapses).
During a flare-up, some people with ulcerative colitis also experience symptoms elsewhere in their body. For example, some people develop:
- painful and swollen joints (arthritis)
- mouth ulcers
- areas of painful, red and swollen skin
- irritated and red eyes
In severe cases, defined as having to empty your bowels six or more times a day, additional symptoms may include:
- shortness of breath
- a fast or irregular heartbeat
- a high temperature (fever)
- blood in your stools becoming more obvious
In most people, no specific trigger for flare-ups is identified, although a gut infection can occasionally be the cause. Stress is also thought to be a potential factor.
Causes
Experts aren’t sure what causes it. They think it might be caused by the immune system overreacting to normal bacteria in the digestive tract. Or other kinds of bacteria and viruses may cause it.
You are more likely to get ulcerative colitis if other people in your family have it.
Treatment
The treatment of colitis depends upon the cause.
For undiagnosed or uncontrolled colitis, the initial therapy (regardless of the cause) is to stabilize the patient’s vital signs and help control pain if needed. Rehydration may be accomplished by mouth. However, for those patients who are markedly dry, who are unable to tolerate fluids by mouth, or have electrolyte abnormalities, intravenous fluids may be required.
Medications are often used to control inflammatory bowel disease and the choice of medication is tailored to the individual patient.
Antibiotics are not commonly used unless a specific bacteria is isolated and treatment is known to shorten the course of the infection.
Over-the-counter medications to treat diarrhea should be used with caution, especially if abdominal pain and fever are present. It is always wise to check with a care provider or pharmacist prior to taking antidiarrheal medications.
Surgery is usually not a treatment option for most causes of colitis.
What foods help soothe colitis flares?
Colitis often is associated with diarrhea, and the body can lose significant amounts of fluid with each episode of diarrhea. Moreover, the colon is inflamed, and it is important to try to “rest” it. Since clear fluids tend to be absorbed mostly in the stomach and small intestine, initially avoiding solid foods and promoting a clear fluid diet may be of help in rehydrating the body and resting the colon.
Changing your diet to reduce symptoms or flares may help soothe the symptoms of the disease, but there is no cure for some forms of colitis.
What foods should I avoid if I have colitis?
Depending on the cause, some people with colitis may find that certain foods bring on or make their symptoms worse. Keeping a food diary may be helpful and then avoid foods that may be associated with worsening symptoms.
The Crohn’s & Colitis Foundation of America recommends avoiding the following foods if you have colitis:
- Greasy or fried foods
- Milk or products containing milk
- Certain high-fiber foods like popcorn, seeds, nuts, and corn
People who are lactose intolerant should avoid dairy products containing lactose. There are a variety of companies (for example, Lactaid and Green Valley Organics) that offer lactose-free products such as milk, yogurt, ice cream, and cottage cheese.
Natural Remedies
Anti-inflammatory diet
This diet aims to eliminate foods that are linked to increased inflammation while adding foods that can fight inflammatory symptoms. Some recommendations include:
- eliminating refined carbohydrates, such as white bread
- avoiding excess consumption of sugar
- avoiding packaged foods and processed meats
- eliminating or reducing the use of trans fats
- eating a Mediterranean diet, which is rich in fruits, vegetables, whole grains, seeds, nuts, and legumes
- eating antioxidant-rich foods, such as blueberries
Phytochemicals
Some chemicals found in plants (phytochemicals) may help reduce symptoms of UC. Research supports a diet that includes:
- apples
- bilberry or huckleberry
- black raspberry
- cocoa
- bael
- green tea
- grapes
- olive oil
- Indian gooseberry
- the edible mushroom Agaricus blazei
Remaining nourished and healthy
Rather than eating or avoiding specific foods, some practical strategies may help reduce the symptoms of flare-ups. These include:
- Drinking plenty of water to remain hydrated, particularly during a bout of diarrhea.
- Drinking electrolyte drinks to maintain electrolyte balance when diarrhea threatens dehydration.
- Taking a calcium and vitamin D supplement to avoid calcium deficiency and bone loss. Many people with UC are calcium or vitamin D deficient.
- Eating several small meals each day, rather than three large ones.
- Eating well and avoiding restrictive diets. Even fast food is preferable to no food at all, particularly in people with UC who are malnourished.
- Eating a low-fiber diet.
- Reducing the consumption of greasy, buttery foods.
- Avoiding milk products. Many people with UC are lactose intolerant.
Lifestyle remedies for UC symptoms
A few lifestyle changes can reduce symptoms of UC. These include:
Therapy
Many people with UC experience depression, anxiety, low self-esteem, or relationship problems. These issues can make it difficult to comply with treatment and may compound the effects of UC. Therapy and support groups can help.
Exercise
Exercise plays a vital role in weight management, which may reduce symptoms of UC. It can also increase energy. Many people feel intense fatigue during a UC flare-up.
