Alzheimer’s disease (AD) is the most common form of dementia among older people. Dementia is a brain disorder that seriously affects a person’s ability to carry out daily activities.
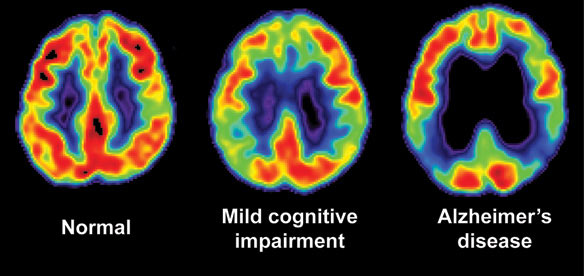
AD begins slowly. It first involves the parts of the brain that control thought, memory and language. People with AD may have trouble remembering things that happened recently or names of people they know. A related problem, mild cognitive impairment (MCI), causes more memory problems than normal for people of the same age. Many, but not all, people with MCI will develop AD.
Contents
Causes
The exact cause of Alzheimer’s disease is unknown, although a number of things are thought to increase your risk of developing the condition. These include:
- increasing age
- a family history of the condition
- previous severe head injuries
- lifestyle factors and conditions associated with cardiovascular disease
Symptoms
The first symptoms of Alzheimer’s vary from person to person. Memory problems are typically one of the first signs of cognitive impairment related to Alzheimer’s disease.
Just like the rest of our bodies, our brains change as we age. Most of us eventually notice some slowed thinking and occasional problems with remembering certain things. However, serious memory loss, confusion and other major changes in the way our minds work may be a sign that brain cells are failing.
The most common early symptom of Alzheimer’s is difficulty remembering newly learned information because Alzheimer’s changes typically begin in the part of the brain that affects learning. As Alzheimer’s advances through the brain it leads to increasingly severe symptoms, including disorientation, mood and behavior changes; deepening confusion about events, time and place; unfounded suspicions about family, friends and professional caregivers; more serious memory loss and behavior changes; and difficulty speaking, swallowing and walking.
Stages
Mild Alzheimer’s disease
As AD spreads through the brain, the number of plaques and tangles grows, shrinkage progresses, and more and more of the cerebral cortex is affected. Memory loss continues and changes in other cognitive abilities begin to emerge. The clinical diagnosis of AD is usually made during this stage. Signs of mild AD can include:
- Memory loss
- Confusion about the location of familiar places (getting lost begins to occur)
- Taking longer than before to accomplish normal daily tasks
- Trouble handling money and paying bills
- Poor judgment leading to bad decisions
- Loss of spontaneity and sense of initiative
- Mood and personality changes, increased anxiety and/or aggression
In mild AD, a person may seem to be healthy but is actually having more and more trouble making sense of the world around him or her. The realization that something is wrong often comes gradually to the person and his or her family. Accepting these signs as something other than normal and deciding to go for diagnostic tests can be a big hurdle for people and families. Once this hurdle is overcome, many families are relieved to know what is causing the problems. They also can take comfort in the fact that despite a diagnosis of MCI or early AD, a person can still make meaningful contributions to his or her family and to society for a time.
Moderate Alzheimer’s disease
By this stage, AD damage has spread to the areas of the cerebral cortex that control language, reasoning, sensory processing, and conscious thought. Affected regions continue to shrink, ventricles enlarge, and signs and symptoms of the disease become more pronounced and widespread. Behavioral problems, such as wandering and agitation, can occur. More intensive supervision and care become necessary, which can be difficult for many spouses and families. The symptoms of this stage can include:
- Increasing memory loss and confusion
- Shortened attention span
- Inappropriate outbursts of anger
- Problems recognizing friends and family members
- Difficulty with language and problems with reading, writing, and working with numbers
- Difficulty organizing thoughts and thinking logically
- Inability to learn new things or to cope with new or unexpected situations
- Restlessness, agitation, anxiety, tearfulness, wandering—especially in the late afternoon or at night
- Repetitive statements or movement, occasional muscle twitches
- Hallucinations, delusions, suspiciousness or paranoia, irritability
- Loss of impulse control (shown through undressing at inappropriate times or places or vulgar language)
- An inability to carry out activities that involve multiple steps in sequence, such as dressing, making a pot of coffee, or setting the table
Behavior is the result of complex brain processes, all of which take place in a fraction of a second in the healthy brain. In AD, many of those processes are disturbed, and these disrupted communications between neurons are the basis for many distressing or inappropriate behaviors. For example, a person may angrily refuse to take a bath or get dressed because he does not understand what his caregiver has asked him to do. If he does understand, he may not remember how to do it. The anger can be a mask for his confusion and anxiety. Or, a person with AD may constantly follow her husband or caregiver and fret when the person is out of sight. To a person who cannot remember the past or anticipate the future, the world can be strange and frightening. Sticking close to a trusted and familiar caregiver may be the only thing that makes sense and provides security.
Severe Alzheimer’s disease
In the last stage of AD, plaques and tangles are widespread throughout the brain, most areas of the brain have shrunk further, and ventricles have enlarged even more. People with AD cannot recognize family and loved ones or communicate in any way. They are completely dependent on others for care. Other symptoms can include:
- Weight loss
- Seizures
- Skin infections
- Difficulty swallowing
- Groaning, moaning, or grunting
- Increased sleeping
- Lack of bladder and bowel control
Near the end, the person may be in bed much or all of the time. The most frequent cause of death for people with AD is aspiration pneumonia. This type of pneumonia develops when a person is not able to swallow properly and takes food or liquids into the lungs instead of air.
Natural Treatment & Remedies
Eating Well
The basic rules of a healthy diet apply to everyone, whether they have Alzheimer’s or not. Build a meal plan that helps your loved one:
- Eat a variety of foods, especially fruits and vegetables, whole grains, lean protein, and low-fat dairy.
- Keep a healthy weight. Proper portion sizes and exercise are a key part of this, too.
- Limit foods with high saturated fat and cholesterol, like fatty meats and fried foods.
- Cut down on sugar.
- Avoid eating too much salt.
- Drink plenty of water.
Omega-3 Fatty Acids
Omega-3s are a type of polyunsaturated fatty acid (PUFA). Research has linked certain types of omega-3s to a reduced risk of heart disease and stroke.
The U.S. Food and Drug Administration (FDA) permits supplements and foods to display labels with “a qualified health claim” for two omega-3s called docosahexaneoic acid (DHA) and eicosapentaenoic acid (EPA). The labels may state, “Supportive but not conclusive research shows that consumption of EPA and DHA omega-3 fatty acids may reduce the risk of coronary heart disease,” and then list the amount of DHA or EPA in the product. The FDA recommends taking no more than a combined total of 3 grams of DHA or EPA a day, with no more than 2 grams from supplements.
Research has also linked high intake of omega-3s to a possible reduction in risk of dementia or cognitive decline. The chief omega-3 in the brain is DHA, which is found in the fatty membranes that surround nerve cells, especially at the microscopic junctions where cells connect to one another.
Ginkgo Biloba
Ginkgo biloba is a plant extract containing several compounds that may have positive effects on cells within the brain and the body. Ginkgo biloba is thought to have both antioxidant and anti-inflammatory properties, to protect cell membranes and to regulate neurotransmitter function. Ginkgo has been used for centuries in traditional Chinese medicine and currently is being used in Europe to alleviate cognitive symptoms associated with a number of neurological conditions.
Exercise
Exercise is good for everyone, and it’s especially important for people with Alzheimer’s disease. It won’t cure the condition, but it can help ease some of its symptoms.
Exercise helps people sleep better and feel more alert during the day, so it can promote a normal day-and-night routine for people with Alzheimer’s. It also can improve mood. Repetitive exercises such as walking, indoor bicycling, and even tasks such as folding laundry may lower anxiety in people with the disease because they don’t have to make decisions or remember what to do next. They also can feel good knowing that they’ve accomplished something when they’re finished.
Personal Care Tips
- Set up a daily routine and stick to it. For example, brush your loved one’s teeth after meals. Or always have baths in the mornings or evenings. Choose the most relaxed times of the day for these tasks.
- Respect her privacy. Close doors and blinds. Cover her with a towel or bathrobe.
- Encourage her to take on as much of her own care as possible. This will give her a sense of independence and accomplishment.
- Keep her abilities in mind. Give her enough time to complete each task — for example, brushing her hair or teeth.
- Encourage and support her. For example, say, “You did a nice job getting dressed today.”
- Tell her what you’re doing before you do it — “I’m going to wash your hair now.”
- If she can dress herself, lay out her clothes in the order she should put them on. It’s best to give her clothing that’s easy to put on, with few buttons.
